This is Your Brain on Opioids
This four-part series explores how opioids affect the brain, in terms of reward and pleasure, neuropathways, and how to recover and repair your brain after opioid addiction.
Part 2: Walking on the Wild Side With NeuropathwaysPart 3: Yes, Your Brain Can ChangePart 4: Self-Care is Brain Repair
Part 1: A Frying Pan of Reward and Pleasure
In the late eighties, the Partnership for a Drug-Free America released its now-iconic series of public service announcements featuring the infamous “This is your brain on drugs” tag line. The basics of the spots were this: an egg is your brain, a hot frying pan represents drugs. Someone cracks the egg into the frying pan. It, well, fries. “Any questions?” a man asks.
Yes. In fact, tons of them, especially since the addiction landscape has changed so much in the last two decades. Still, it was a good start and the heart of the message remains true: simply put, drugs alter your brain. Obviously it’s a little more complicated than the ads implied, and as the opioid epidemic grows and treatment modalities evolve, it’s more important than ever to understand what, exactly, opioids do to our brains–and the long-term effects of opioid use.
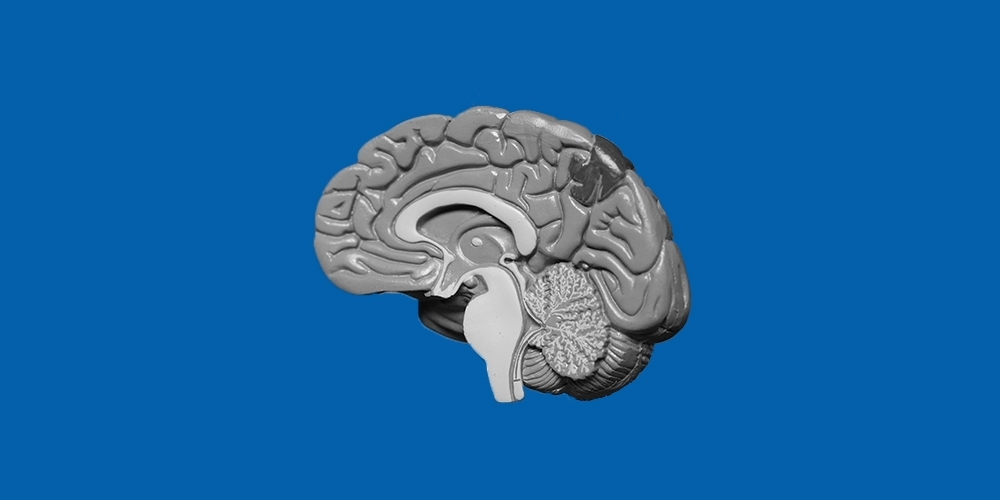
Turns out, it’s all about neurotransmitters, which is incredibly helpful unless you fell asleep in science class and don’t remember what a neurotransmitter is. Really a neurotransmitter is just a chemical that controls communication in your brain. Your brain releases neurotransmitters from a nerve cell and transfers it to another nerve cell and so on, sort of like a brain game of telephone except the message remains the same. All of our basic functions require neurotransmitters to do their jobs, as nerve cells communicate with one another and share information.
“Your brain releases neurotransmitters from a nerve cell and transfers it to another nerve cell and so on, sort of like a brain game of telephone except the message remains the same.”
In fact, you’re probably at least familiar with the names of two of our neurotransmitters: serotonin and dopamine. The first helps control important functions like mood, sleep, and appetite. That’s why a lot of antidepressants are designed to increase our serotonin levels. Dopamine is also linked to how we think and feel, as well as to our brain’s pleasure and reward centers.
In our systems, we also have neurotransmitters that are called endogenous opioids, which just means opioids that our body produces internally. You’ve probably heard of endorphins, especially in reference to exercise or a runner’s “high.” (Here’s an interesting fact: the term endorphins actually comes from “endogenous morphine.)
These neurotransmitters are our natural stress and pain fighters, but our bodies can’t produce enough of these organic opioids to save us from feeling severe or chronic pain or from suffering from extreme stress. Which is where taking opioids comes in. Opioids basically act like those naturally-occurring neurotransmitters but in much larger quantities. They attach to your brain’s natural opioid receptors and go to town. Opioids flood the brain’s reward and pleasure systems, signaling our brains to block out the pain, lower our stress, and calm us down.
“Opioids flood the brain’s reward and pleasure systems, signaling our brains to block out the pain, lower our stress, and calm us down.”
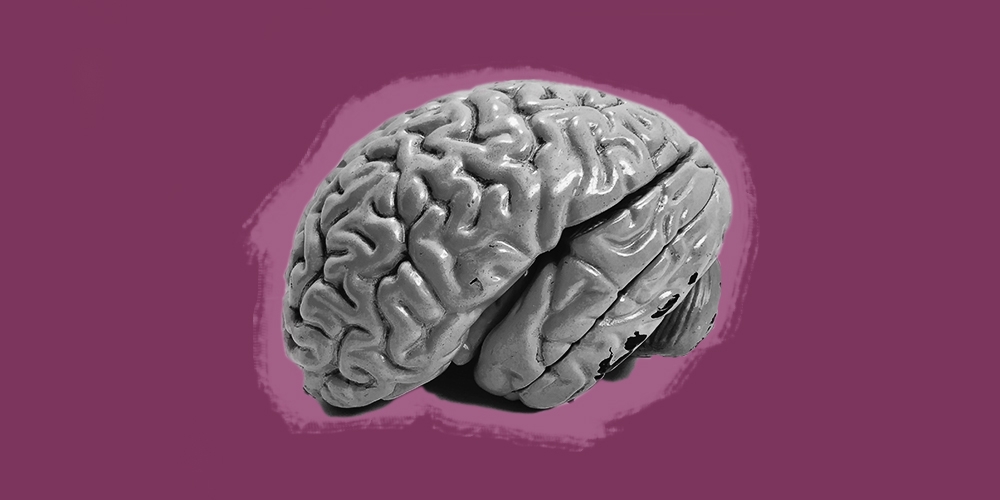
Over time, adding these opioids –whether in the form of heroin or morphine or codeine– actually alters our brain chemistry. According to the Journal of Neuroscience, “the repeated use of opiates induces alterations in neurotransmitter and neuropeptide systems that regulate incentive–motivation and stress–responsiveness. Increasing evidence indicates that the dysregulation of these systems underlies the compulsive use and loss of control of drug-taking that characterizes opiate and other addictions.” Got that?
Just in case that wasn’t clear, here’s the bottom line: repeated opioid use changes our brains at the cellular level. Once altered, our brains literally respond differently to stress and pain. We need more. Our natural opioids aren’t nearly enough. Long-term opioid use also alters the way our brains respond chemically to triggers. We can be triggered to use simply by being around the people, places and/or objects associated with our drug use. So it’s not a matter of willpower or character weakness that we’re triggered when we get around old haunts–it’s an actual alteration in our brains as a result of sustained opioid use.
It’s all pretty daunting, but the good news is that just as opioids have changed our brains, we have the ability to heal them. And that’s what we’ll explore next.
Your Brain on Opioids, Part 2: Walking on the Wild Side With Neuropathways
Opioids change the brain, but the good news? Your brain can heal.
Now that we’ve taken a look at how opioids affect the brain in the long run, let’s focus a bit on the good news–we have the ability to help our brains heal and to develop new healthy, habits. It’s time to talk neuroplasticity.
While we might associate the word “plastic” with hardness and durability, in the scientific sense it really means that something has the ability to flex and change. So when scientists talk about neuroplasticity, they’re talking about how much our brain remains changeable. It’s about the flexibility we have to develop new skills, acquire new knowledge, and create new habits. Neuroplasticity is how we learn to speak a new language or play a new instrument–and it’s also what recovery from opioids depends on.
“Neuroplasticity is how we learn to speak a new language or play a new instrument–and it’s also what recovery from opioids depends on. ”
It all comes down to neuropathways, or neural pathways. These are actual trails created in our brain over time by repetition and habit. When we roll out of bed and sleepwalk through our morning routine almost automatically, that’s thanks to the neuropathways we’ve created by doing the same thing every morning.
A common analogy is to think of neuropathways as actual walking paths or hiking trails. It’s easy to imagine how walking the same path over and over becomes so familiar that you can do it with hardly any conscious thought. When we abuse opioids over a period of time, through sustained use, we create a well-worn pathway in our brain so that it becomes almost an unconscious habit to use. Your brain knows this route. It knows the twists and turns. It’s easy to follow.
When we choose recovery, and we choose to do something other than using drugs, we are actually attempting to change our brain structure. Recovery requires us to create new neuropathways in our brain, but the cool thing is we can do it. Just as we changed our brain through the habit of addiction, we can help heal it through sustained and repeated healthy recovery habits. Which, frankly, is about as rad as it gets.
“Recovery requires us to create new neuropathways in our brain, but the cool thing is we can do it.”
Waking up each day and deciding not to use is a brand new way of doing things for your brain. To go back to the walking path analogy, you’re forging a brand new trail in the wilderness. The ground is rocky and uncertain, there are discouraging obstacles in the way, and everything is unfamiliar and uncomfortable.
In short, it’s hard. We’re rewiring our brains and it’s tough work. (Especially when our brains keep reminding us how much easier it would be just to fall back on that old neuropathway of addiction.) It takes time and practice to really form that new path, to make it clearer, more familiar, and less uncomfortable to navigate.
But if we stick with it–especially if we can just get through those first difficult days when our brain is frustrated and confused–it gets easier over time because those recovery neuropathways get stronger and deeper every time we choose not to use.
So how do we do it? How do we start to change our brains? Next time, we’ll take a look at some specific tips and tools that can help us heal our brains and create those neuropathways that can carry us away from opioid addiction and into a new, healthy way of living.
Ready to get building new neuropathways? Check out the next section of this series:
Your Brain on Opioids, Part 3: Yes, Your Brain Can Change
After opioid addiction, your brain can recover and repair.
Now that we’re all well on our way to becoming brain scientists, let’s focus a little bit on how, exactly, we heal our minds by building new neuropathways. Like a lot of things in recovery, it’s simple enough in theory, but challenging in practice.
(Read Your Brain on Opioids, Part 2: Walking on the Wild Side With Neuropathways)
In a nutshell, we create new neuropathways by establishing and practicing new habits. The more we repeat them, the more ingrained those neuropathways become.
Here are four key elements of the process.
1. Motivation and intention
It all starts here, with our motivation for getting clean, our intentions, and our goals. Motivation is a powerful thing—without it, none of our recovery efforts can find footing. At the outset, we have to prep our brains for change by spending some time identifying what it is we want to do. It’s essential that we’re really clear with ourselves about our goals, and that we acknowledge and harness all the motivation we can for kicking opioids in the rear.
“Motivation is a powerful thing—without it, none of our recovery efforts can find footing.”
2. Get honest
It’s tough, but necessary, to take a good, hard look at our addiction to opioids and what it has done to our lives. We have to be honest about how it’s ruined our relationships, finances, health, etc. And it’s not enough just to think about it! We have to put pen to paper (or fingers to keyboard), and see it all in black and white.
3. Recognize triggers
As we’ve learned, our brains are hardwired to respond to the people, places, and things that we associate with our addiction, triggering our desire to use. No matter how strong-willed or tough we think we are, our brains have other plans. We have to take a clear look at the lives we’ve built, and identify the specific people, places, and things that are triggers for us. For the road ahead, we’re going to have to be our own trigger cops, staying vigilant and aware at all times. At Workit Health, a big part of early recovery is learning to recognize triggers, and to handle the cravings that they cause.
4. Change our responses to addictive thoughts/patterns as they arise
So we acknowledge what triggers us … then what? Instead of using, we … don’t use, right? That’s all there is to it? In some ways, recovery really does boil down to that difference. But it’s so much easier said than done. There’s a saying in recovery circles that the only thing you have to change is everything—which isn’t super comforting, but there is certain amount of truth in there.
“Even the smallest changes help our brains adapt.”
(Read Part 1: This is Your Brain On Opioids)
Unfortunately, we can’t just decide that we’ll avoid triggers and then our addiction will be fixed. The brain doesn’t work that way—nor does the world always cooperate in helping us avoid them. Those old neuropathways associated with using are deep. Again, we have to distract our brains by creating new neuropathways. We do that every time we make a new, healthier choice. Part of the Workit program is learning to kick old auto thoughts to the curb, and welcoming their opposites, called antidotes, into our life.
Paving a new road is exhausting, so it may be less daunting to think of it as laying one little paving stone after another. Even the smallest changes help our brains adapt. If you’re used to getting up and sitting at the counter with a cup of coffee while you take your first pill of the day, do something different in recovery. Sit at your kitchen table and drink milk instead. Or even drink your coffee out of a different mug. Along with big decisions (such as not using), all of these small decisions confuse your brain and help break the connections that trigger cravings. They add up.
Creating new neuropathways is a long process, and we have to remind ourselves that we’re actually retraining our brains. That requires care and dedication, plus a fair amount of sweat and tears. There are also other things we can do, healthy habits and supportive activities we can introduce into our lives to help our bodies support these brain changes—and that’s what we’ll look at next, in part 4:
Your Brain on Opioids, Part 4: Self-Care is Brain Repair
Recovering from opioid addiction? Heal your brain with self-care.
The first three parts of this series focused on our brains – how we start to heal them in recovery. Equally important are the ways we can take care of our bodies in recovery, ways that also support our efforts to heal our brains and maintain their neuroplasticity. Just tuning in? Get the scoop on how opioids change our brains, and how we can work to change them back, starting with the first part in this series: This Is Your Brain On Opioids.
Exercise
Our bodies go through a lot when we’re using. Helping them recover is daunting, but moving our bodies is essential to both physical and mental health. Studies have shown how exercise can improve our moods, sleep and concentration, as well as reduce anxiety and stress. Exercise is also how we re-train our brains to release and recognize our natural endorphins. We don’t have to run marathons. We can start with some gentle yoga or even a ten-minute walk. The point is to get our bodies moving again. And, as with everything we’ve been discussing, we want to create a habit, a new neuropathway, so that exercise becomes part of our everyday lives and our recovery.
Meditation
Some of us may be as intimidated by the idea of mediating as we are by the idea of exercising regularly. We tend to over-complicate the simple idea of sitting quietly and being mindful. Research shows that meditation changes the way our brains work for the better, and some studies are focusing on how it aids specifically with addiction recovery. Don’t be afraid of it. There are tons of resources online, including some great apps, to help you get started. Or check to see if there are any meditation classes offered in your area.
Cognitive Behavior Therapy
Cognitive behavior therapy is a therapy modality that’s been around since the late 1960s. Under the guidance of a qualified therapist, it helps us recognize the patterns of behavior we need to change and gives us the support to make those changes. Which, as you know all too well by now, helps create and maintain positive neuropathways in our brains. CBT has been proven to be a very useful tool in recovery addiction and relapse prevention by helping us understand how we act and react, why we do so and what we can do differently in the present.
Nutrition
Almost all of us neglected self-care while we were actively using, especially when it came to eating right, creating nutritional and vitamin deficits that make it harder for the brain to do its work. Eating well helps heal both our bodies and our minds. (Nutrition is becoming an increasing focus for rehab centers, and a study by the National Center for Biotechnology Information found that rectifying nutritional deficiencies in opiate addicts increased the effectiveness of methadone intervention.)
But it doesn’t take a brain scientist to recognize how we should be eating in recovery: less sugar and processed carbohydrates, more protein, and more fresh fruits and vegetables. By eating properly and eating regularly, we are redeveloping the habits (hello, neuropathways!) of self-care that get so easily lost in the chaos of addiction.
Sleep
We all know how much addiction messes with our sleep patterns and in early recovery, establishing normal sleeping cycles may be as frustrating as searching for a pot of gold at the end of a rainbow. Still, it’s crucial that we try to re-establish good sleep habits and retrain our brains. Setting a regular bedtime and adhering to it is a great start. Don’t get too frustrated if sleep seems elusive at first. As with all things in recovery, it takes time and effort to establish good habits.
Play
Now for the fun stuff! A healthy brain depends on neuroplasticity and we’re both relying on it and improving it with the new habits we’re creating in recovery. It’s also essential to keep our brains on their proverbial toes with some fun approaches. Doing crossword puzzles or Sudoku, playing trivia games, learning a new language or taking up a new hobby are all great ways to support our newly alert, newly recovering brains on their journey back to health.