Medical Professionals Experience Substance Use Disorder
Intelligence, training, and subject knowledge are no defense against addiction. An estimated 868,000 members of the medical profession struggle with substance use disorder.

Medical Professionals Experience Substance Use Disorder
Intelligence, training, and subject knowledge are no defense against addiction. An estimated 868,000 members of the medical profession struggle with substance use disorder.
Medical professionals face unique challenges in treating their mental health and addiction.
Doctors, nurses, and other members of healthcare professions are, to some extent, put on a pedestal in our society. Medical professionals are highly educated, highly skilled, and carry a professional authority that many admire. Despite this occupational awe, these professionals experience substance use disorder (SUD) at similar rates to the rest of the population. Neither education nor skill offers protection against substance use disorder. Healthcare workers are often unwilling to seek treatment due to stigma and fear of professional sanctions.
Prevalence of substance use disorders among medical professionals
On the whole, physicians tend to engage in healthier habits than the general population, but this does not extend to substance use. It is estimated that 10-12% of doctors will develop an SUD during their careers. Rates are similar for nurses and pharmacists. This is not only a source of personal concern for the medical professionals affected, it is also a serious public health issue. Healthcare workers hold positions of authority and responsibility, and when impacted by SUD, can do great harm.
Occupational challenges facing medical professionals
Working in the medical field brings unique pressures and challenges that often become risk factors for SUD.
- Stress
Medicine is a high-pressure field. Patient care never really stops, and work hours are often long. Many in the healthcare industry are shouldering both the weight of patient outcomes and the burden of institutional pressure to work more and faster. Many in the field cope with this stress by self-medicating.
- Access to substances in the workplace
One challenge that is unique to the medical field is access to medications and controlled substances. Working in a pharmacy, doctor’s office, or hospital often provides access to medications that laypeople don’t have.
- Physical pain
People outside the healthcare industry often have no idea how physically demanding many medical roles are. From nursing assistants all the way up to surgeons, healthcare professionals deal with heavy lifting, long hours on their feet, repetitive stress, pulled muscles, and more … often contributing to chronic pain. Managing physical pain is cited as one of the most common reasons medical professionals misuse drugs.
- Confidence in self-medicating
Years of medical training and professional experience can lull many into a false sense of security. After all, if they know how meds affect a person, surely they can avoid the dangers. Some call this fallacy “pharmaceutical invincibility.” Unfortunately, history shows that neither medical degrees nor experience protect against substance use disorder. Addictive substances affect highly knowledgeable brains in the same ways they affect others.
- Compassion fatigue
Compassion fatigue is a risk among healthcare professionals. This is a secondary traumatic stress disorder that can develop from helping others, leading to symptoms of anger, depression, and apathy. Like other mental health concerns, compassion fatigue can lead to substance misuse in an attempt to escape or manage it.
Obstacles that keep medical professionals from seeking help
Despite experiencing SUD at the same rates as laypeople (some studies say higher), medical professionals are often loathe to seek treatment. Here are a few of the most commonly cited concerns:
- Stigma
Reputation can feel like everything in the medical field, and many are unwilling to risk their professional reputation if others learn that they are in treatment for an SUD. The other side of this coin is that by not seeking treatment, they make it more likely that their active addiction or substance use will be discovered.
- Disciplinary action and professional sanctions
Despite the existence of health professional monitoring programs and health professional recovery programs that help medical professionals, many in the field fear the consequences if they are discovered to have an SUD. They are concerned with the loss of license to practice, and with employers levying professional consequences.
- Distrust of the treatment
It is a conundrum that many medical professionals make the worst patients. Their own knowledge can make it difficult to trust in the expertise of others to prescribe them care, especially if they have not been able to vet the clinicians or counselors who are treating them. This is especially true if they have any disagreement with their own healthcare provider about the course of treatment.

Signs of substance use disorder among medical professionals
According to the American Medical Association Journal of Ethics, some signs of SUD or addiction in healthcare professionals include:
- Attendance issues: being late to appointments, having more absences, unknown whereabouts
- Unusual rounding times, either very early or very late
- Increase in patient complaints
- Increased secrecy
- Decrease in quality of care; making careless medical decisions
- Incorrect or incomplete charting or writing of prescriptions
- Decrease in productivity or efficiency
- Increased conflicts with colleagues
- Increased irritability and aggression
- Smell of alcohol; overt intoxication; needle marks
- Erratic job history
Getting help for addiction
It’s estimated that only one in ten people who need treatment for addiction receive it. Doctors, nurses, pharmacists, and other medical professionals are often among the majority who struggle alone, whether out of fear of professional consequences, distrust of the treatment, or peer pressure that normalizes substance use while dismissing help. Despite these concerns, healthcare workers deserve support to get their lives back. And taking care of themselves will make them better equipped to heal and care for others.
Treatment can offer support that will help stabilize addiction recovery and care for the other mental health concerns that might be tied to substance use. While many medical professionals do not feel able to go away to an in-person rehab for thirty or sixty days, the rise in telemedicine has made it possible to receive effective, science-backed addiction treatment via phone or computer. Workit Health is secure, WCAG-accessible, and a SOC 2 Type II compliant program—an industry leader in telehealth care.

For yourself, your loved ones, and your patients
The stigma around substance use disorder keeps many from seeking treatment, and this is especially true among medical professionals. With licensure and professional reputation on the line, we understand this reluctance. But substance use disorder is serious and often progressive, with consequences that affect yourself, your loved ones, and your patients.
You deserve expert care that can help you recover.

Start your recovery
No waiting rooms, no judgment, just easy streamlined virtual recovery care
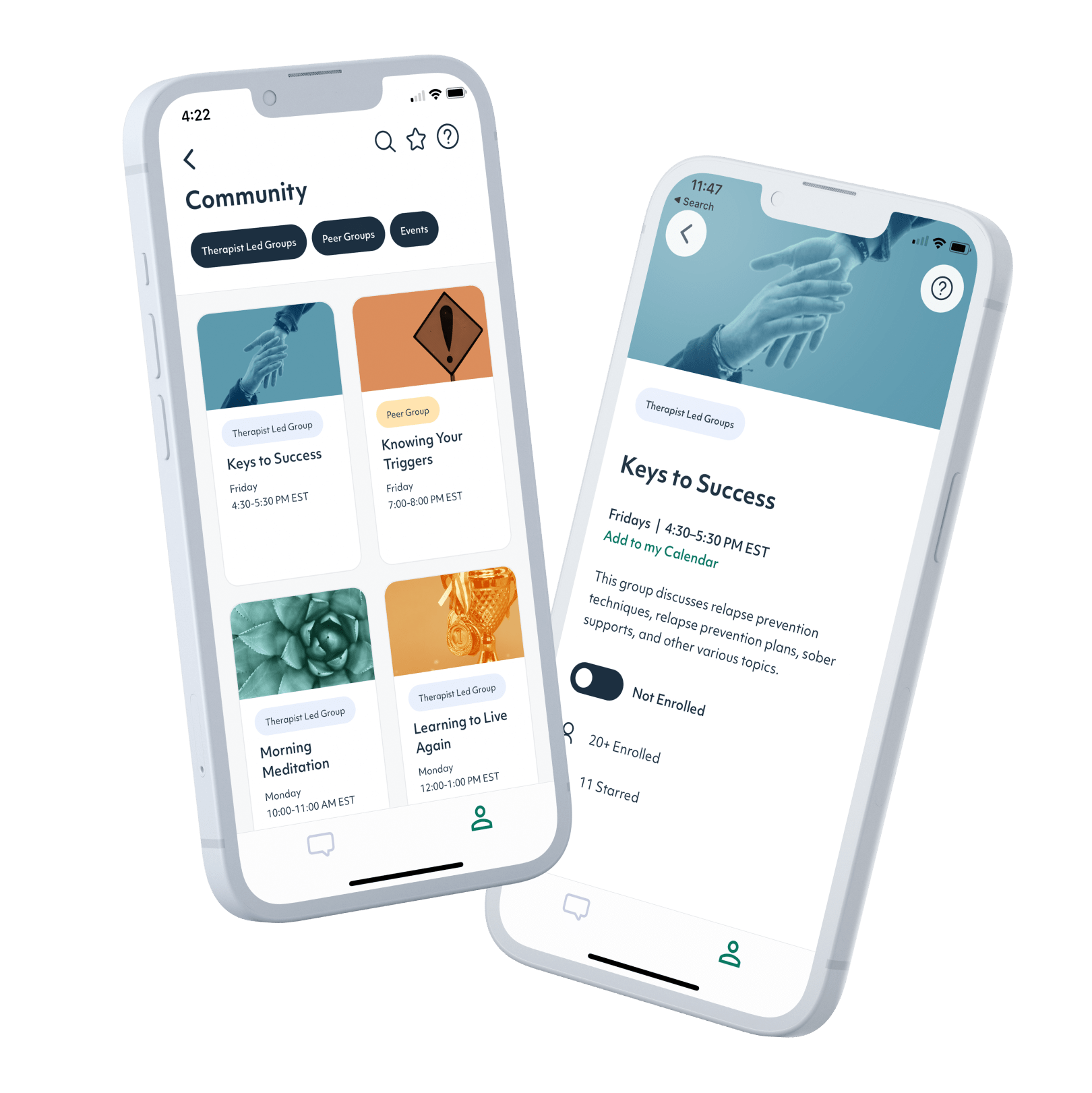
1. Sign up
It only takes a few minutes. Download our app and answer a few questions about your treatment goals, then schedule your first appointment.
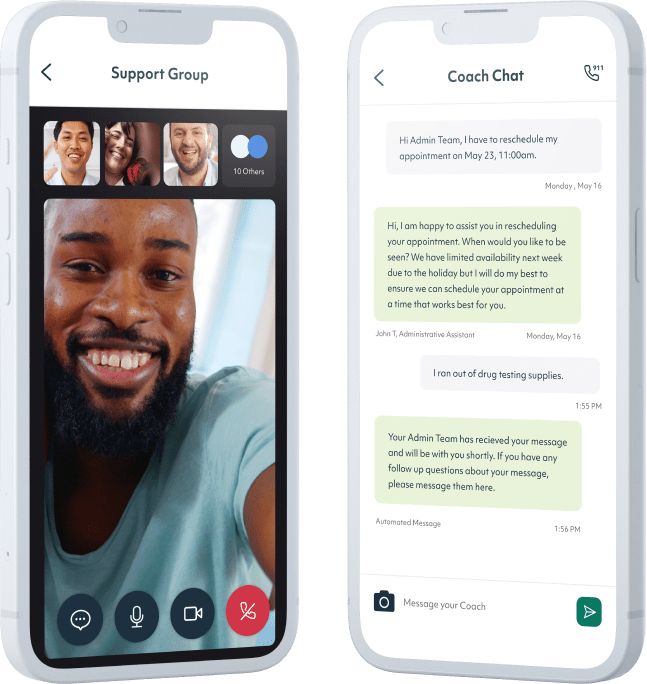
2. Meet with a provider
Meet with a licensed provider via a secure video appointment to set your recovery goals and establish your treatment plan.
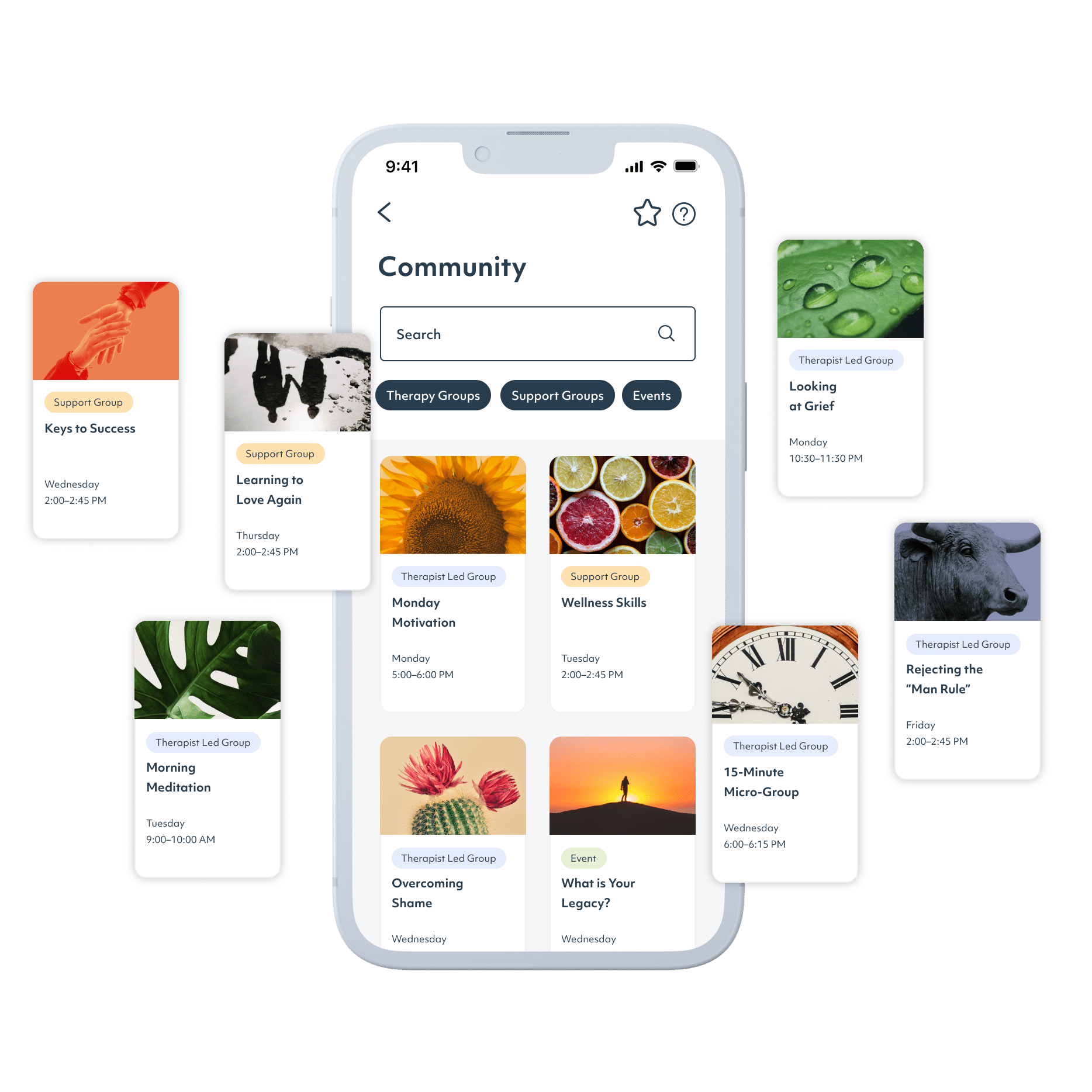
3. Get ongoing support
Shared Medical Appointments, recovery groups, and online community provide support and help you build skills to navigate life sober.
No waiting rooms, no judgment, just easy streamlined virtual recovery care
Trusted by major insurance providers
Citations
1. Pew Research Center (2019). “Trust and Mistrust in Americans’ Views of Scientific Experts”
2. Bass, K., & McGeeney, K. (2012). U.S. Physicians Set Good Health Example. Gallup. https://news.gallup.com/poll/157859/physicians-set-good-health-example.aspx
3. Kenna, G. A., & Wood, M. D. (2004). Prevalence of Substance Use by Pharmacists and Other Health Professionals. Journal of the American Pharmacists Association, 44:6, 684-693.
https://doi.org/10.1331/1544345042467281.
4. Merlo, L.J., & Gold, M.S. (2008). Prescription Opioid Abuse and Dependence Among Physicians: Hypotheses and Treatment. Harvard Review of Psychiatry. 16:3, 181-194. https://doi.org/10.1080/10673220802160316.
5. Kenna, G. A., & Lewis, D. C. (2008). Risk factors for alcohol and other drug use by healthcare professionals. Substance abuse treatment, prevention, and policy, 3:3. https://doi.org/10.1186/1747-597X-3-3
6. Ross, S. (2003) Identifying an impaired physician. Virtual Mentor. 5:12, 420-422. https://doi.org/10.1001/virtualmentor.2003.5.12.cprl1-0312.





