Opioid withdrawal is scary, but there is help
Tap on a topic to learn more about opioid withdrawal symptoms and treatment.
What does "opioid withdrawal" really mean?
Opioids like pain pills, heroin, and fentanyl change the way certain receptors in the brain. Prescribed opioid medication is effective for short-term pain relief, but long-term use can cause physical dependence and increased tolerance, or the need to use more opioids to feel the same effects. Once physical dependence is developed, stopping opioids can cause many withdrawal symptoms.
Although opioid withdrawal is very uncomfortable, the good news is that there are medications that can help you feel more comfortable as you detox, and reduce the risk of overdose or relapse in the future.
In this guide, Workit experts explain what opioid withdrawal symptoms feel like, how you can use a clinical opiate withdrawal scale to evaluate your level of withdrawal, and how opioid agonist treatment with medication like buprenorphine or methadone can help you.
What is opioid withdrawal?
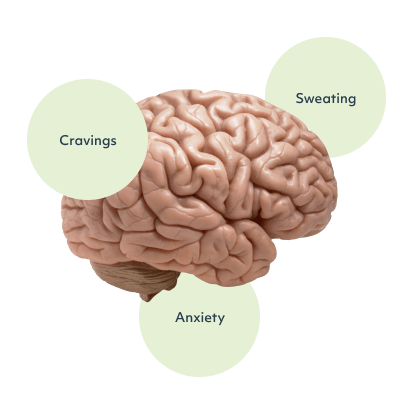
Long-term opioid use affects a chemical in your brain called dopamine. Dopamine is called a pleasure chemical and is associated with many activities that make us feel good or relieve pain. Eating chocolate, petting a fluffy animal, or exercising all can cause an increase in dopamine. Dopamine is part of our brain’s reward circuitry, which reinforces pleasurable activities. If something feels good, your brain is trained to anticipate it and want to do it more.
All types of addiction affect the brain’s reward circuitry. Opioid drugs flood the brain with dopamine, causing pain relief, relaxation, and euphoria. When you take opioids long-term, your brain and body begin to produce less natural chemicals and rely on the drugs you’re consuming. Withdrawal occurs when your body responds to the absence of the drug.
What are common opioid withdrawal symptoms and how long do they last?
Different opioids last in your body longer, with short-acting opioids like codeine, hydrocodone, oxycodone, and oxymorphone causing a more rapid onset of withdrawal symptoms than opioids that stay in your system longer, like methadone and fentanyl. Your healthcare provider can help you evaluate your use, and what opiate withdrawal symptoms you can expect.
72 hours after your final dose of opioids:
- Chills
- Fever
- Body aches
- Diarrhea
- Insomnia
- Muscle pain
- Nausea
- Dilated pupils
One week after your final dose of opioids:
- Tiredness
- Sweating
- Body aches
- Anxiety
- Irritability
- Nausea
Two weeks after your final dose of opioids:
- Depression
- Anxiety
- Irritability
- Restlessness
- Trouble sleeping
- Cravings
Symptoms that begin two weeks after use are often called post-acute withdrawal syndrome and may linger for several months. It’s vital in this stage to work with health care professionals to receive support for your mental health as well as possibly receive pharmacotherapies for the management of cravings.


What medications help with opioid withdrawal?
Prescription opiate withdrawal treatments
- Suboxone: Most common brand name for buprenorphine/naloxone, an opioid agonist-antagonist combination designed to reduce withdrawal symptoms and manage cravings long-term. This unique medication has a ceiling effect that prevents the euphoria caused by other opioids and is FDA-approved for the treatment of opioid use disorder. Workit Health offers 100% telemedicine Suboxone treatment in certain states. Other brand names of buprenorphine/naloxone commonly prescribed includee Zubsolv, Bunavail.
- Methadone: Used to treat pain and in maintenance programs to taper down from other opioids. When methadone is prescribed for drug abuse, it is dispensed by Opioid Treatment Programs certified by SAMSHA, commonly called methadone clinics.
- Clonidine: Clonidine is a blood pressure medication that can help with opiate withdrawal, as well as withdrawal from cigarettes, alcohol, or benzodiazepines. It works by affecting your body’s nervous system, as well as counteracting low blood pressure caused by withdrawal.
- Zofran: Zofran, the brand name for the generic anti-nausea medication ondansentron, is a prescription medication that can help with nausea and vomiting caused by opiate withdrawal.
Over-the-counter treatments for opioid withdrawal syndrome
- Imodium: Imodium (brand name for the generic over-the-counter anti-diarrhea medication loperamide) can help with the stomach issues caused by opiate withdrawal. We recommend taking it only as directed and never taking more than is instructed on the label.
- Dramamine: Over-the-counter anti-nausea meds such as Antivert, Bonine, and Dramamine can help with nausea caused by withdrawal. These are commonly offered for motion sickness.
- Advil or Tylenol: For achy muscles, take acetaminophen (like Tylenol) or ibuprofen (like Advil). A hot bath or a slow walk can also work wonders.
Is fentanyl withdrawal different than withdrawal from other opioids?
Fentanyl is a highly potent opioid that is used in medical settings to manage pain but is also taken illicitly. Because of its potency, many street drugs are cut with fentanyl. Although fentanyl is very dangerous, and fentanyl addiction is on the rise, fentanyl withdrawal can be treated with medications used to treat withdrawal from other opioids. Because the half-life of illicit fentanyl is often unknown, it’s important to rely on an opiate withdrawal scale, like the COWS score or the SOWS-Gossop score, to understand your level of withdrawal.


Post-acute withdrawal syndrome
Many people experience withdrawal symptoms for a prolonged period of time. This extended process of withdrawal is called post-acute withdrawal syndrome (PAWS). PAWS often recurs periodically in episodes of a few days and can fluctuate in severity. These episodes can persist for up to two years. People who go through full withdrawal (not mitigating it with one of the prescription treatments listed above) are more likely to develop PAWS.
Common symptoms of PAWS:
- Irritability
- Cravings
- Anxiety or panic
- Insomnia
- Difficulty with cognitive tasks (remembering things, learning, problem-solving)
PAWS symptoms can be triggered or made more severe by stressful situations, but they can also recur without any obvious triggers. If PAWS causes you distress, speak with your healthcare provider.
Has my opioid use become a problem?
Take our opioid self-assessment to check on your use. This tool should not be used as a replacement for a clinical diagnosis.






