Ready to detox off heroin or pain pills? We give you basic info about buprenorphine/naloxone, commonly called by popular brand name, Suboxone.
Making the decision to detox from opiates is described by Workit staff member and former user Kali, as “an easy choice, a logical decision, (that) has suddenly become the most difficult of my life.” Maybe you’re reading this article because you are in the process of making that decision, or maybe you already have. If so, congratulations! But with this decision comes many questions. Fear not, that’s what we are here for. Let us take some of that weight off your shoulders.
1. Is Suboxone an opiate?
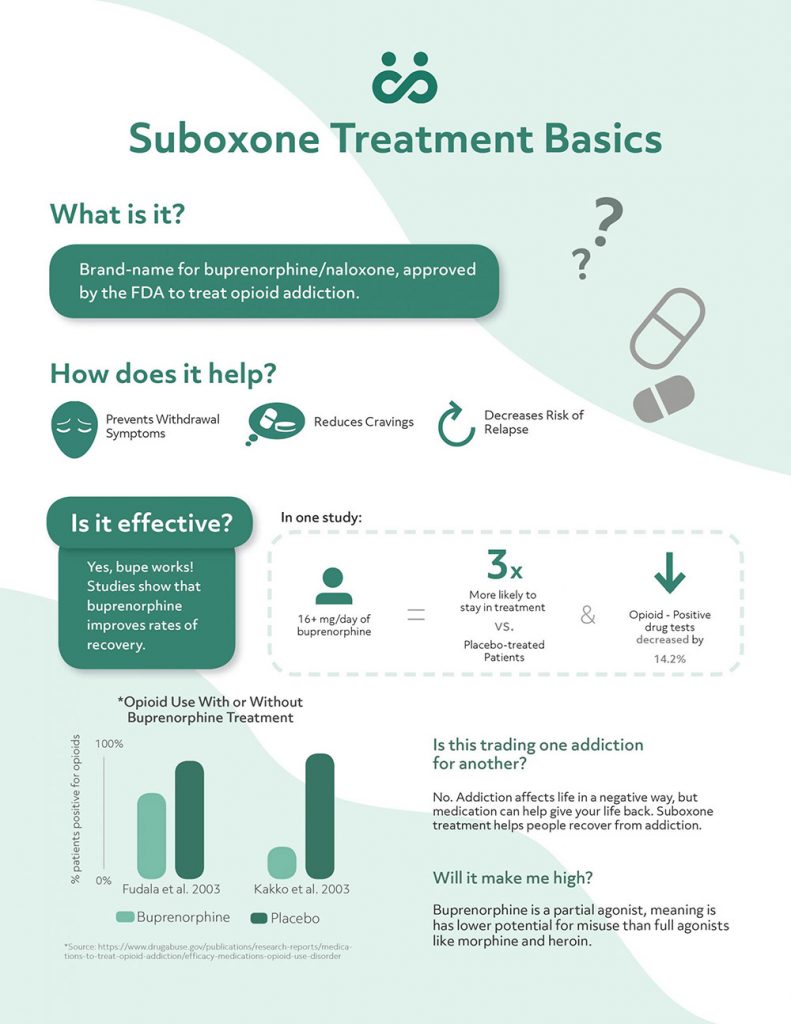
Quite literally, yes it is¹. Heroin operates by binding opioid receptors in your brain, spinal cord, or stomach. This receptor binding causes euphoric pain relief. The main ingredient of Suboxone is buprenorphine, and it operates by occupying those same receptors, therefore competing with anything (like heroin) that can bind these receptors. Any substance than binds those receptors and produces even the slightest high, is by definition, an opioid². These substances include heroin, morphine, methadone, buprenorphine, hydrocodone, and oxycodone. Buprenorphine produces a minimal high.
Bottom Line: Yes, Suboxone is an opiate, but it produces a minimal high.
2. So what’s the difference between an opiate and an opioid?
An opiate is a drug derived from opium. Synthetic opiates have been referred to as opioids, but now the definition of opioid has expanded. In the medical community, opiate still tends to refer to substances directly derived from opium. At Workit, we have recovered addicts on staff who used the terms interchangeably in the past, and we continue to do so to speak to the community.
Bottom Line: At one time, opiates were drugs made from opium and opioids were synthetic opiates. Now? The two terms are interchangeable.
3. But isn’t the purpose of these drugs to help me stop taking opiates?
Yes, most certainly. Suboxone operates by binding the opioid receptors to prevent withdrawal while producing a minimal high, therefore helping to prevent against any recreational use. This binding helps individuals stop their heroin or pill habit by reducing cravings. With time, Suboxone doses can be lessened and lessened to the point where an individual is no longer reliant on any opiates. Consider Suboxone as the safer intermediate in the middle of your path to recovery.
Bottom Line: Taking Suboxone can help you get off of traditional full-agonist opiates while avoiding bad withdrawal. It can also prevent relapse and many people chose to stay on Suboxone as a maintenance drug.
4. What’s the difference between Suboxone and buprenorphine?
Good question! Suboxone contains buprenorphine and naloxone. Buprenorphine is a partial agonist, meaning it occupies the same opioid receptors as heroin but doesn’t produce the same high. Naloxone (better known as Narcan) is an antagonist, meaning it blocks the receptors and produces absolutely no high. The naloxone prevents Suboxone from being severely abused. Buprenorphine alone does have abuse potential because it can produce a high.
Bottom Line: Suboxone is buprenorphine with naloxone added to it to prevent severe abuse potential.
5. What’s the difference between Suboxone and methadone?
Drugs called full agonists bind opioid receptors at a high frequency and result in heavy euphoric feelings. Methadone is a full agonist. Partial agonists also bind these receptors, but their effects are less pronounced. Buprenorphine is a partial agonist. Finally, antagonists bind the receptors and turn them off by preventing anything else from binding. Suboxone is 80% buprenorphine, so it is mostly a partial agonist, but it’s also 20% naloxone. The naloxone component exists to prevent users from abusing the drug to achieve highs.
You can safely transition from methadone to Suboxone. At Workit Health, we recommend a slow taper to 30mg of methadone for 2 weeks before beginning Suboxone treatment.
Bottom Line: Methadone works differently in your brain, and has a higher misuse potential than Suboxone.
6. How long will it take me to get off of Suboxone?
The scientific results of this topic are somewhat mixed. One study shows that a full Suboxone taper is very difficult with only 9% of the study’s participants fully completing the taper and remaining opiate free³. However, another study found great success with the tapering process with 60% of participants prescription opiate free after 40 months⁴.
In Workit Clinic, each member’s dose and duration on medication is planned by their medical team.
In Workit Clinic, each member’s dose and duration on medication is planned by their medical team.
In addition to medication, members enjoy access to educational content and messaging with a coach team for recovery support. Why? Because your addiction doesn’t take breaks; and neither do we.
Bottom Line: Tapers vary in length, and always need to be completed under medical care. Contact Workit Clinic if you’re ready to make a change.
7. What are the side effects of long term Suboxone use?
Some individuals decide to continue to use Suboxone in the long term. One study has shown that Suboxone (compared to other opioid medicines) can help a person regain their once productive and social states⁵. Another study found that Suboxone use lead to forms of minor emotional blunting⁶. If consumed with alcohol or benzodiazepines, the outcome can be fatal. In some cases, individuals have reported headache, pain, withdrawal syndrome, infection, insomnia, back pain, and constipation. It has been shown that, in general, a switch to Suboxone results in an improvement in overall health.
Bottom Line: As with any drug, Suboxone has side effects. But it can help you kick an opiate addiction.
8. Will Suboxone show up on a drug test?
It will not show up on a standard drug test, unless your employer specifically tests for buprenorphine, the main ingredient in Suboxone. Remember that just because Suboxone is an opiate, however, doesn’t mean it’s unsafe or not okay to take as prescribed.
Ali Safawi goes into this in more detail in an article where he explains, “The opioid ingredient in Suboxone, buprenorphine, will not show up in an opioid drug test unless you are taking a multi-panel test which specifically tests for buprenorphine. Even then, if you are being prescribed Suboxone, you shouldn’t have to worry about a positive test buprenorphine test.”
9. What can happen if I decide to just stop taking opiates all together?
A sudden cessation of opiates can result in withdrawal. Nausea, muscle cramping, depression, agitation, anxiety, and opiate cravings characterize withdrawal. While the withdrawal process itself may not be life-threatening, it will lead to intense opiate cravings, which could lead to an overdose scenario. Suboxone prevents the withdrawal from happening and will decrease the cravings.
Bottom Line: Anyone who has tried to quit opiates cold turkey knows this bottom line already. Opiate withdrawal can be rough. Suboxone might be able to help.
To again quote our staff member and recovered opiate addict: “A pill habit lands you in a world where it’s all under control, until it’s suddenly, desperately not.” The first step to regaining control is making the decision to detox. One of the most important parts of this action is to make sure you do it in a safe, clinically effective manner.
-
Lutfy, K., & Cowan, A. (2004). Buprenorphine: A Unique Drug with Complex Pharmacology. Current Neuropharmacology, 2(4), 395–402. https://doi.org/10.2174/1570159043359477
-
Opiate vs. Opioid – What’s the Difference? (n.d.). Retrieved July 16, 2017, from https://opium.com/derivatives/opiate-vs-opioid-whats-difference/
-
Weiss, R. D., Potter, J. S., Fiellin, D. A., Byrne, M., Connery, H. S., Dickinson, W., … & Hasson, A. L. (2011). Adjunctive counseling during brief and extended buprenorphine-naloxone treatment for prescription opioid dependence: a 2-phase randomized controlled trial. Archives of general psychiatry, 68(12), 1238-1246.
-
NIDA. (2015, November 30). Long-Term Follow-Up of Medication-Assisted Treatment for Addiction to Pain Relievers Yields “Cause for Optimism”. Retrieved from https://www.drugabuse.gov/news-events/nida-notes/2015/11/long-term-follow-up-medication-assisted-treatment-addiction-to-pain-relievers-yields-cause-optimism on 2017, July 12
-
Fudala, P. J., Bridge, T. P., Herbert, S., Williford, W. O., Chiang, C. N., Jones, K., … & Ling, W. (2003). Office-based treatment of opiate addiction with a sublingual-tablet formulation of buprenorphine and naloxone. New England Journal of Medicine, 349(10), 949-958.
-
Hill, E., Han, D., Dumouchel, P., Dehak, N., Quatieri, T., Moehs, C., … & Blum, K. (2013). Long term Suboxone™ emotional reactivity as measured by automatic detection in speech. PLoS one, 8(7), e69043.