Measurement-based care (MBC) sounds kind of boring, but it’s really valuable. MBC refers to the use of regular, systematic assessments to get a person’s perspective on their own progress and recovery. At Workit Health, we send out these assessments to members through our app, asking them to report on their experiences. We usually call these assessments “Health Checks” when we talk about them.
Completing a Health Check one time gives us a look at how a member is feeling, but the real power of MBC comes when they fill out the same Health Check regularly over the course of their treatment.
Here at Workit Health, we currently use three assessments:
Substance Use Recovery Evaluator (SURE)
There are many assessments out there that seek to measure an individual’s progress in recovery. What makes the SURE assessment unique is that it was designed with input from people in recovery. It includes items about substance use, self-care, relationships, resources, and outlook on life. By addressing these five factors, SURE aims to represent a unified measure of recovery.
How often is it taken? Workit Health asks our members to complete the SURE every month.
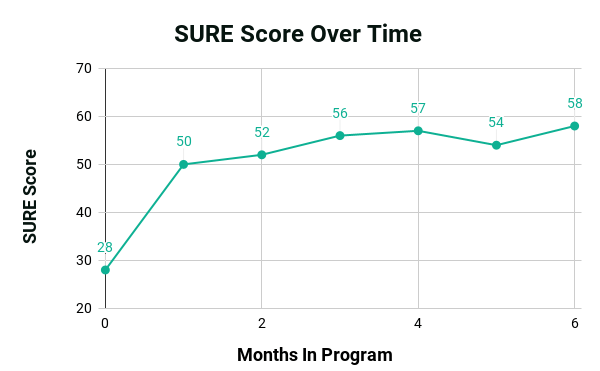
What do the results mean? Scores range from 21 to 63, and a higher score on SURE indicates a higher level of recovery. When looking at a graph of SURE scores over time, a line pointing up represents improving recovery over time. People who identify as being in recovery typically have a score of 45 or higher. Here’s an example of one member’s SURE scores over time. This member reported improving recovery, with a period of life difficulties in their fifth month. We’ll use the same member’s responses to illustrate the other Health Checks.
Patient Health Questionnaire-9 (PHQ-9)
The PHQ-9 is a questionnaire specifically used to screen for depression and suicidal ideation, and to gauge the severity of symptoms of depression. It consists of nine questions that ask an individual to reflect on the previous two weeks and how they’ve been feeling during that time.
How often is it taken? Workit Health asks all of our members to take the PHQ-9 when they begin treatment and every six months after that. However, for folks whose results show symptoms of depression, we ask them to complete it once a month.
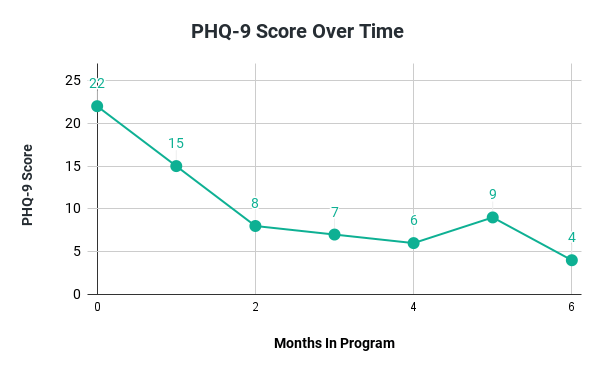
What do the results mean? A higher score on the PHQ-9 indicates greater symptoms of depression. Scores range from 0-4—indicating no or minimal depression—all the way up to 20-27—which indicate severe depression. When looking at a graph of PHQ-9 scores over time, a line pointing downward represents an improvement (reduction) in depression symptoms. Here’s an example of one member’s PHQ-9 scores over time. This member reported decreasing depression symptoms, with a period of increased depression during that tough time in their fifth month.
General Anxiety Disorder-7 (GAD-7)
The GAD-7 is a questionnaire that’s used to screen for and measure the severity of general anxiety disorder symptoms. It consists of seven questions that ask an individual to look back at how frequently they’ve experienced anxiety symptoms over the previous two weeks.
How often is it taken? Workit Health asks all of our members to take the GAD-7 when they begin treatment and every six months thereafter. For folks whose results show symptoms of anxiety, we ask for it to be completed once a month.
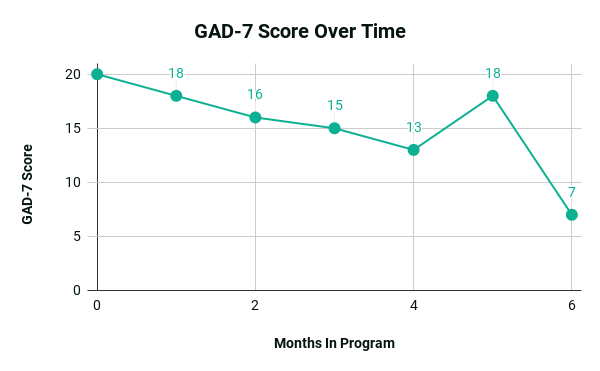
What do the results mean? A higher score on the GAD-7 indicates greater symptoms of anxiety. Scores range from 0-4—indicating no or minimal anxiety—up to 15-21—which indicate severe anxiety. When looking at a graph of GAD-7 scores over time, a line pointing downward represents an improvement (reduction) in anxiety symptoms. Here’s an example of one member’s GAD-7 scores over time. This member reported decreasing anxiety symptoms through their treatment, with a period of increased anxiety coinciding with some struggles (reported in the SURE Health Check) during their fifth month.
Why is measurement-based care good for our members?
Workit Health tries to ensure that any new tasks we ask members to complete are to their benefit (not just busy work). Here are a few important ways that Health Checks are good for members:
- MBC helps clinicians to know whether your treatment is working. In the same way that other medical problems are tracked through laboratory tests or X-rays and other imaging, Health Checks help your care team know how you are doing and whether your treatment is helping.
- MBC can be a warning sign when things are getting hard. Just as it can be difficult to recognize our progress, it can also sometimes be hard to spot the red flags when we’re in a tough situation. After all, how often do we wave off our struggles with, “I’m fine, I’ll manage” … right up to the point that we can’t manage? Health Checks mean that our members are telling their care team how they feel (in clear, quantifiable ways) on a regular basis, so difficulties can be identified and addressed in a timely manner.
- MBC makes sure members have a voice in their care. Because Health Checks are self-reported, they ensure that members get a chance to express how they’re feeling and doing. Some people find it difficult to speak up in an appointment, but Health Checks are low-pressure and completed on the member’s own time.
How does measurement-based care help providers?
Workit Health providers are always striving to provide better care to their members. Here are some important ways that MBC is helpful for providers:
- MBC offers consistency in Health Checks. Having regular, systematic Health Checks with their members means that providers can optimize their time in appointments (both 1:1 and Shared Follow-up Appointments).
- MBC allows for personalized care and resources. It’s important that providers know how their members are doing, so they can offer the best care. Health Checks give providers greater awareness of how members are doing, so they can adapt each member’s treatment and connect them to additional resources, as needed.
- MBC identifies trends in the larger group. While Health Checks are extremely useful for individual care, they also help identify trends across the member community. This can help Workit Health recognize which aspects of the program are working best, and which could be adjusted to better meet members’ needs.
The MBC assessments we use are such helpful tools, for Workit Health and for our members.